Mothers
Infant Pulse Oximeter for Monitoring Newborn Oxygen Levels Safely
Feb 12 • 6 min read

Table of Content
Newborn breathing can look irregular especially during sleep, feeding, or crying and for many parents, even a brief pause in breathing can feel alarming. While most oxygen fluctuations in healthy babies are normal, understanding what is truly safe versus potentially dangerous is essential.
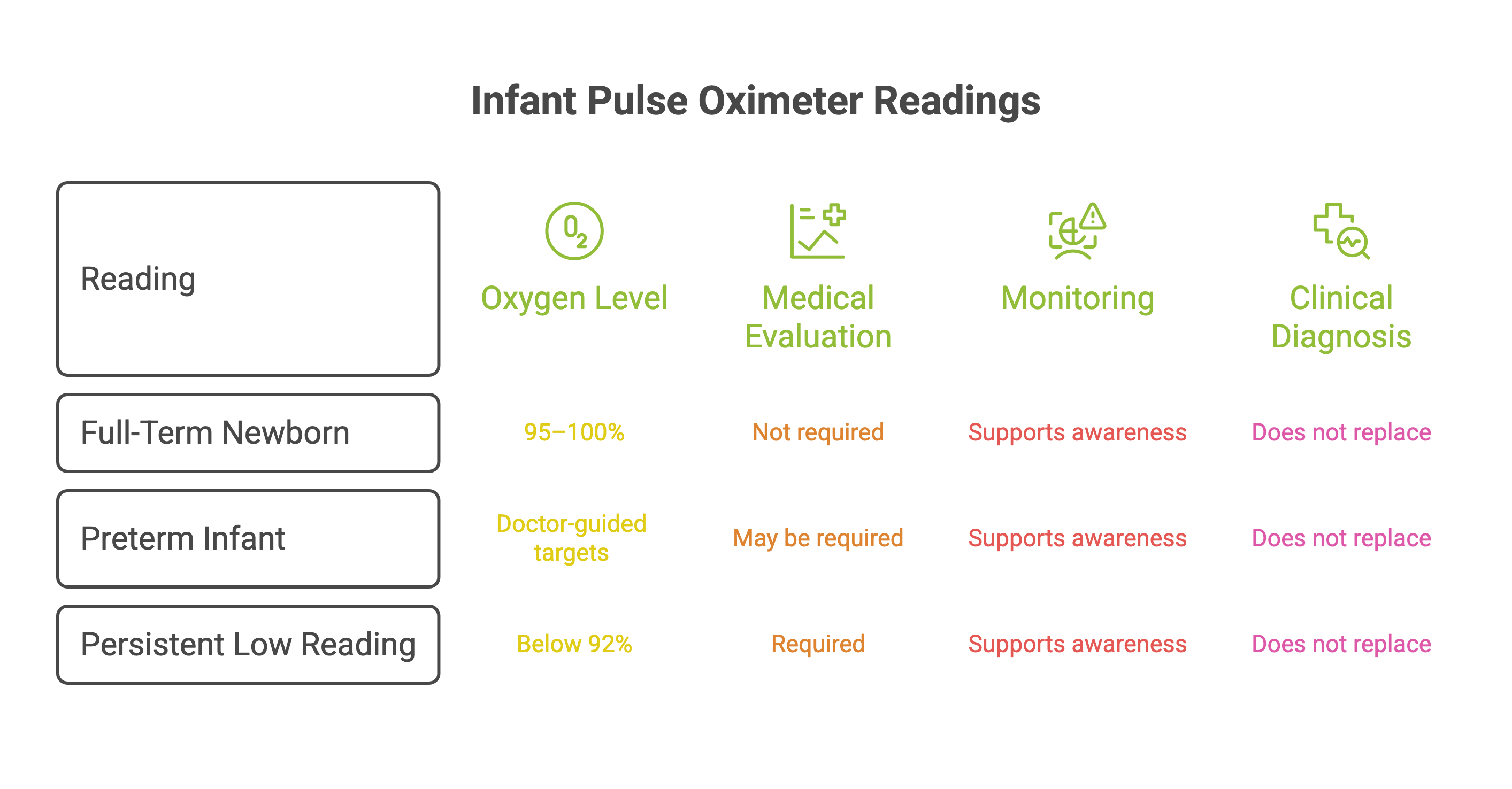
A normal oxygen level in full-term newborns typically ranges between 95–100% (SpO₂). Readings that remain consistently below 92% may require medical evaluation. Because newborn physiology differs significantly from adults, accurate measurement depends on using a device specifically designed for infants.
An infant pulse oximeter is a non-invasive, neonatal-calibrated device that measures oxygen saturation (SpO₂) and pulse rate in babies. When used responsibly and alongside pediatric guidance, it helps parents monitor trends, recognize early warning signs of hypoxia, and make informed decisions without unnecessary panic.
Understanding how these devices work and when monitoring is truly needed empowers safer, more confident newborn care.
What Is an Infant Pulse Oximeter?
An infant pulse oximeter is a device specifically designed to measure blood oxygen saturation and pulse rate in newborns and infants. It uses light-based sensors placed on a baby’s small limb commonly secured around the foot for better stability to provide real-time oxygen readings.
Full-term newborns typically maintain oxygen levels between 95–100%
Preterm infants may have slightly lower doctor-guided targets
Persistent readings below 92% require medical evaluation
Monitoring supports awareness but does not replace clinical diagnosis.
How Pulse Oximeter Works in Newborns
Pulse oximetry works by emitting red and infrared light through the skin to measure how much oxygen is attached to hemoglobin. Oxygen-rich and oxygen-poor blood absorb light differently, allowing estimation of oxygen saturation levels.
This technology is widely used in hospitals and adapted for neonatal care.
Because newborns have:
Delicate skin
Smaller blood vessels
Developing lungs
Lower perfusion levels
Devices designed specifically for infants provide more reliable readings than adult versions.Continuous monitoring may help detect silent hypoxia ,low oxygen levels without obvious visible symptoms.
Why Oxygen Monitoring Matters in Babies
Infants can experience rapid physiological changes, especially if premature or recovering from illness. Early detection of oxygen drops can prevent complications.
Monitoring may be recommended for:
Premature infants
Babies recovering from respiratory distress
Congenital heart conditions
Bronchiolitis
Sleep-related breathing concerns
Post-NICU discharge care
When interpreted correctly, oxygen monitoring supports early medical intervention and safer pediatric care.
Understanding Hypoxia in Infants
Hypoxia refers to low oxygen levels in body tissues. In newborns, prolonged hypoxia can affect brain development, organ function, and overall growth.
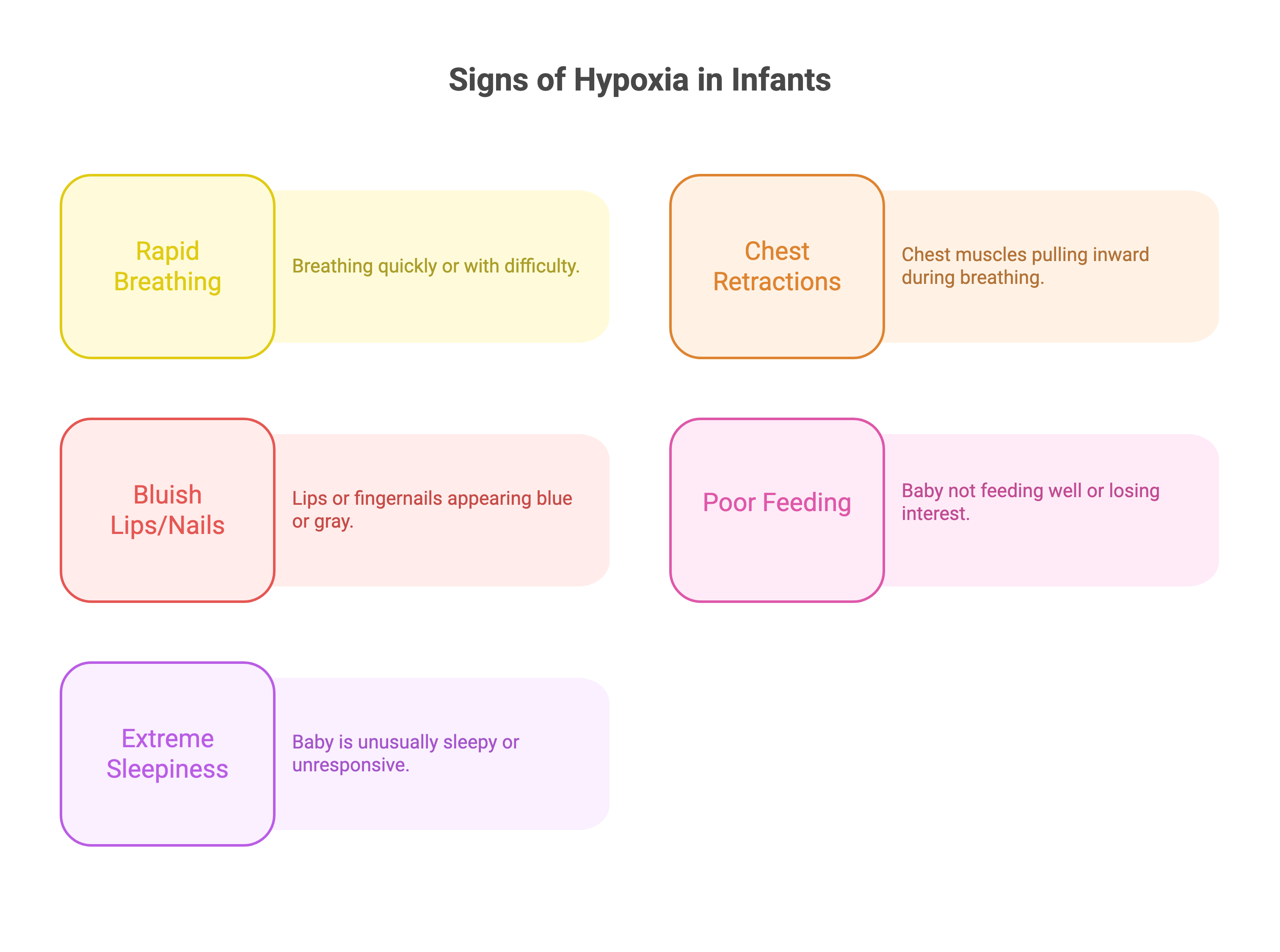
Signs of possible hypoxia include:
Rapid or labored breathing
Chest retractions
Bluish lips or nails
Poor feeding
Extreme sleepiness or lethargy
If symptoms are present, seek medical care immediately, even if device readings appear borderline.
Normal Oxygen Levels in Newborns
Normal newborn oxygen (SpO₂) levels are typically 95–100% after the first few minutes of life. Consistent readings below 90–92% may signal breathing or heart concerns and need medical attention.
How to Check Oxygen Levels Correctly
Secure the sensor properly on the baby’s limb (commonly the foot for better stability)
Ensure the baby is calm and still
Wait for the reading to stabilize
Observe trends rather than reacting to a single number
Always interpret readings alongside visible symptoms.
Infant Pulse Oximeter vs Finger Pulse Oximeter: What’s the Differernce?
The Device is specifically designed for infants, allowing sensors to fit onto small feet or hands for proper and secure oxygen level monitoring. A finger pulse oximeter is specifically designed to fit adult hands, but pulse oximeters for infants may provide faulty results due to improper size fit.
Summary:
Foot oximeters are designed for babies and tend to provide more reliable readings for infants. Finger pulse oximeters are generally meant for adults and older children and are not recommended for newborn home monitoring.
Clinical research indicates that device accuracy can vary depending on how the device is designed and calibrated for infants. Studies like:
PMID: 40355254 — Diagnostic accuracy of an over-the-counter infant pulse oximeter
PMID: 37072015 — Accuracy of a wireless pulse oximeter in preterm or low birth weight infant.
Continuous Monitoring vs Spot Checks
Continuous monitoring tracks vital signs continuously, giving us immediate data, trends, and alarms if levels change. Spot checks measure the level just once. Although helpful, they only give us admittedly limited information. Continuous monitoring allows quicker intervention, better safety tracking, and more peace of mind—particularly with newborn or home care.
Key Features to look for in the Best Infant Pulse Oximeter
When selecting an pulse oximeter, prioritize:
Neonatal-specific sensor design
Stable fit on small limbs
Motion resistance
Accurate low-perfusion detection
Clear alerts and display
Pediatric validation
Accuracy and safety should come before cost considerations.
Safety & Medical Reliability
Pulse oximetry is a clinically validated method widely used in hospitals. However, home monitoring should always complement pediatric supervision.
Parents should:
Use devices as directed
Maintain routine pediatric visits
Avoid self-diagnosis based solely on numbers
Seek medical care when symptoms are present
Responsible use builds confidence while ensuring safety.
when to consult a Doctor Immediately
Seek urgent care if:
Oxygen levels remain below 90–92%
Baby struggles to breathe
Lips or nails turn blue
Feeding decreases significantly
Baby appears unusually lethargic
Trust your instincts. If something feels wrong, consult a healthcare professional.
Conclusion

As a parent, it’s often the small changes that worry you the most. A slight bluish tint to the lips (cyanosis), a faster heartbeat than usual (tachycardia), difficulty breathing (dyspnea), or quietly dropping oxygen levels (hypoxia) can feel overwhelming especially when you’re not sure what’s normal.
An infant pulse oximeter helps you make sense of those moments. When you understand normal oxygen ranges and know what certain signs mean, you’re better prepared to respond calmly and seek help when it truly matters.
Navam Baby Monitor by Janitri is designed with that reassurance in mind. It provides real-time oxygen saturation and pulse readings using a soft, skin-safe sensor that’s gentle on delicate newborn skin. With clear alerts to signal abnormal readings, it helps you notice subtle changes early without adding unnecessary stress. It’s not about replacing your pediatrician; it’s about feeling a little more confident in between visits.
Because when it comes to your baby, even a little extra reassurance can mean everything. Learn more about Navam Baby Monitor and see if it feels right for your family.
Is an infant pulse oximeter different from a finger pulse oximeter?
Yes. An infant pulse oximeter is designed specifically for newborn physiology and small limbs. Finger pulse oximeters are made for adults and may provide inaccurate readings in babies, especially premature or low-birth-weight infants.
Can an infant pulse oximeter detect silent hypoxia?
It may help identify low oxygen levels even when symptoms are not obvious. However, it should not replace professional medical evaluation or diagnosis.
What is hypoxia in babies?
Hypoxia occurs when a baby’s body does not receive enough oxygen. Prolonged hypoxia can affect brain and organ development. Early detection and medical evaluation are critical to prevent complications.
Is it normal for a baby’s oxygen level to drop during sleep?
Yes, brief and mild oxygen dips can occur during normal sleep cycles. However, sustained low readings or drops accompanied by breathing difficulty should be assessed by a doctor.